It is not because of Alcohol!
Love your liver. Is that even a tall order?
This is a zoom into NAFLD, as promised in my previous article (Live It Up, Liver!).
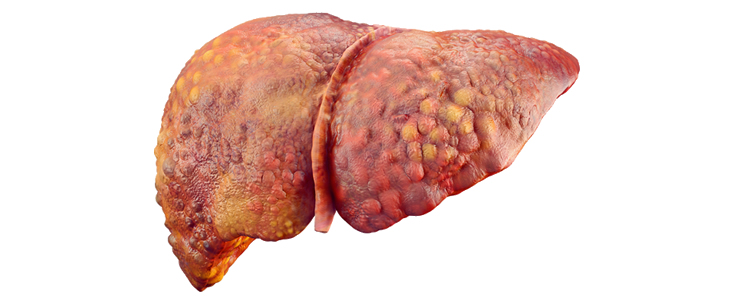
Non Alcoholic fatty liver disease
As the name implies, the disease is not because of alcohol.
Non Alcoholic Fatty Liver Disease (NAFLD) is one of the most common causes of liver disease in the United States; about 30-40% of adults have NAFLD. Moreover, it is also a growing problem in some other countries/continent, making it a major cause of liver disease worldwide [1]. It is an umbrella term for a variety of liver disorders affecting people who do not drink or drink a little alcohol [2].
It is normal to have fat in less than 5% of the liver cells. However, if the fat makes up 5-10% of your liver’s weight, then it is a fatty liver disease.
NAFLD has two main types:
-
- Simple fatty liver – also called “steatosis”. There is fat build up with no or little inflammation or liver cell (hepatocyte) damage. It usually does not worsen to cause serious liver complications or damage.
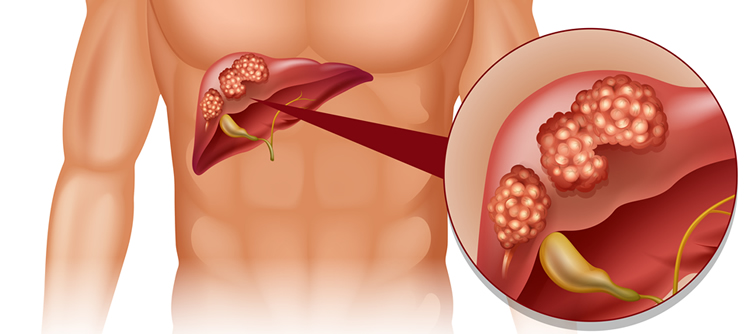
- Non-alcoholic steatohepatitis (NASH) – a condition where there is fat build up, inflammation and cell damage in the liver. It can cause fibrosis (thickening and scarring), cirrhosis (non-living scar tissue replaces normal liver tissue) or liver cancer.
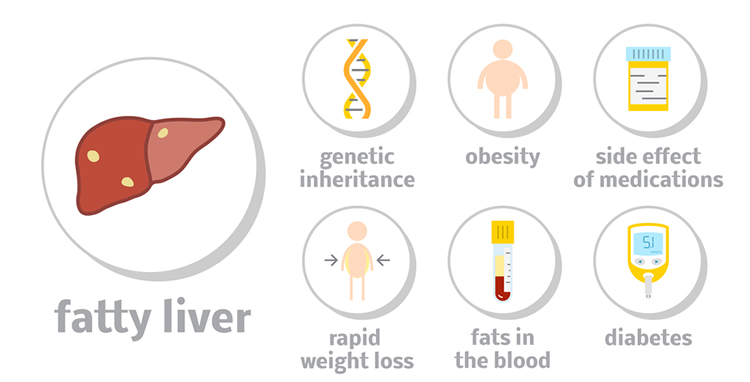
What can cause NAFLD?
The following factors put a person at higher risk for NAFLD [2]:
- High cholesterol (high total cholesterol, high LDL (“bad cholesterol”), or low HDL (“good cholesterol)
- High levels of triglycerides in the blood
- Obesity, particularly when fat is concentrated in the abdomen
- Polycystic ovary syndrome
- Type 2 diabetes/ insulin resistance
- Metabolic syndrome – doctors define metabolic syndrome as the presence of any three of the following: high levels of triglycerides in the blood, low levels of HDL cholesterol in the blood, high blood pressure, higher than normal blood glucose levels, large waist size [3].
- Underactive thyroid (hypothyroidism)
- Underactive pituitary gland (hypopituitarism)
- Smoking
- Studies are still looking into the role of genes in NAFLD development.
Fast Fact: NAFLD has also been observed in children and teen-agers. According to the National Institutes of Health, close to 10% of U.S. children ages 2 to 19 have NAFLD.
Less common causes of NAFLD and NASH include [3]:
- Disorders that cause the body to use or store fat improperly
- Rapid weight loss
- Certain infections, such as hepatitis C
- Certain medicines, such as amiodarone (used to treat irregular heartbeat), diltiazem (used for chest pain & hypertension), glucocorticoids (used for inflammatory conditions), highly active antiretroviral therapy (used for HIV patients), methotrexate (used to treat certain cancers), synthetic estrogens, tamoxifen (used to treat and prevent breast cancer), valproic acid (used for seizures, mental conditions, etc)
- Exposure to some toxins
What are the symptoms of NAFLD and NASH?
Nonalcoholic fatty liver disease usually presents no signs and symptoms. But when it does, they may include [2]:
- Enlarged liver
- Fatigue
- Pain in the upper right abdomen
Possible signs and symptoms of nonalcoholic steatohepatitis and cirrhosis include [2]:
- Yellowing of the skin and eyes (jaundice)
- Abdominal swelling (ascites)
- Enlarged blood vessels just beneath the skin’s surface
- Enlarged breasts in men
- Enlarged spleen
- Red palms
- Fatigue
- Unexplained weight loss
- Weakness
Note: Please consult with your physician if you have any health concern or symptoms.
How can one prevent NAFLD? [4]
It’s as easy as 1-2-3!
- Maintain a healthy weight
- Eat a healthy diet (include Vitamin C-rich foods, avoid fatty and sugary foods)
- Exercise regularly
- Limit alcohol intake (or just continue to avoid alcohol if you don’t drink)
- Only take medicines that you need and follow dosing recommendations.

Treatments for NAFLD:
According to a study [5], the disease starts from excess calorie intake and lack of physical activity, the modification of unhealthy lifestyles is the foundation of any prevention and treatment strategy while drugs should remain a second-line of treatment.
A. Diet and lifestyle
Healthy diet
Try to have a balanced diet high in vegetables & fruits but low in fat (especially saturated and trans-fat), sugar and salt. Eating smaller portions of food can also help.
Reducing caloric intake, increasing soy protein and whey consumption, and supplement of monounsaturated fatty acids, omega-3 fatty acids and probiotics have preventive and therapeutic effect [7].Try to avoid soft drinks; avoid fruit juices that contain a lot of fructose and minimize fast food intake. Lessen intake of red and processed meats, increase intake of fish [9].
Exercise (or maintain physical activity) regularly
Target at least 150 minutes of moderate-intensity activity per week (e.g. walking or cycling). All types of exercise can help improve NAFLD. However, recent studies show that a combination of aerobic exercise and weight training is more effective than an aerobic exercise alone [8].
Weight management/ weight loss
At least 3-5% of weight loss achieved by low calorie diet alone or in combination with physical activity and behavioral modification, usually reduces fatty liver [7]. 7-10% weight loss is required to help reduce liver inflammation [8]. Weight management is important in NAFLD patients. Doctors recommend gradually losing 7 percent of your body weight or more over the course of 1 year as rapid weight loss through very low calorie diet or fasting can make NAFLD worse [10]. Healthy diet and exercise are key to weight management/weight loss.
Management of risk factors
Management of health in people with high blood glucose or diabetes and high cholesterol is upheld.
Alcohol intake
Any type or amount of alcohol consumption should be avoided in NAFLD patients.
Stop smoking
In people with NAFLD and who smoke cigarettes, stopping can help reduce the risk of problems such as heart attacks and strokes.

B. Medications
Currently, there is no approved medicine to treat NAFLD and NASH. Many studies are being done about medications, like pioglitazone (Actos), a medicine for type 2 diabetes. Doctors may recommend vitamin E for people who have NASH and don’t have diabetes or cirrhosis.
Some doctors will recommend vaccination against Hepatitis A and B.
C. Liver Transplant
For patients who have cirrhosis due to NASH, liver transplantation may be an option [6].
Note: If you are a NAFLD or NASH patient, please consult with your doctor first before trying any dietary supplements, complementary and alternative medicine or herbs.
Relevant and recent researches/updates on NAFLD:
A study [11] suggested that portion (called LBP) of wolfberry/ goji berry, garlic-derived compounds, red grape–derived resveratrol, and milk thistle–derived substances offer unanticipated and great health benefits without obvious adverse effects in NAFLD treatment although more detailed and long-term studies are needed for their applications. The study also suggested that green tea components are useful in the prevention of NAFLD.
“In studies of people with NAFLD, those who reported drinking coffee had less liver damage than those who drank little or no coffee. It’s not clear how coffee may influence liver damage or how much coffee you’d need to drink in order to benefit. [2]”.
Several studies have suggested positive relationship between regular coffee consumption and its protective effects on the liver. It was also shown to reduce risk of fibrosis in NAFLD patients.
A recent study [12] in 2017 stated that that the gut microbiome (see previous article: Mind Your Tummy) represents a significant environmental factor contributing to NAFLD development and progression. Probiotics may have a helpful role in the management of NAFLD through a many possible mechanisms (e.g. obesity induction & inflammatory response triggering).
With time, there will be more research updates on how to prevent and treat NAFLD and NASH.
Conclusion
With the worldwide rise of obesity comes the emergence of NAFLD. NAFLD is also associated with other disease conditions including diabetes, cardiovascular diseases, and metabolic syndrome. Common denominators of these conditions are diet, physical activity, weight management and lifestyle practices. Therefore, we should consider these factors to prevent or treat these diseases.
Improve Your Liver Health NOW!

Do you have stubborn fat? Are you stuck on a plateau where no matter what you do, you just can’t lose weight?
LivLean, our best-selling blend of 15 all-natural ingredients, is clinically proven to promote liver health. LivLean Supports:
- Liver Health & Detoxification
- A Healthy Metabolism
- Immune Function
- Healthy, Normal Blood Sugar Levels
CLICK HERE TO LEARN MORE ABOUT LIVLEAN.
References
- Younossi Z.M., Koenig, A.B., Abdelatif, D., Fazel, Y., Henry, L. & Wymer ,M.. (2016). Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology, 12(38): 6098–6101. DOI: 10.1002/hep.28431.
- Mayo Foundation for Medical Education and Research. (2017). Nonalcoholic Fatty Liver Disease. Retrieved from http://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/home/ovc-20211638
- The National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. (2016). Symptoms and Causes of NAFLD and NASH. Retrieved from https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/symptoms-causes
- American Liver Foundation. (2017). NAFLD Non Alcoholic Fatty Liver Disease. Retrieved from http://www.liverfoundation.org/abouttheliver/info/nafld/
- Caporaso, N., Morisco, F., Camera, S., Graziani, G., Donnarumma, L. & Ritieni, A. (2012). Dietary approach in the prevention and treatment of NAFLD. Frontiers in Bioscience, 17:2259-2268. DOI: 10.2741/4049
- National Health Service (UK). (2017). Non-alcoholic Fatty Liver Disease (NAFLD). Retrieved from http://www.nhs.uk/conditions/fatty-liver-disease/Pages/Introduction.aspx
- Fan, J.G., Cao, H.X. (2013). Role of diet and nutritional management in non-alcoholic fatty liver disease. Journal of Gastroenterology and Hepatology, 4:81-7. DOI: 10.1111/jgh.12244
- Oh, H., Da, W.J., Saeed, W.K. & Nguyen, M.H. (2016). Non-alcoholic fatty liver diseases: update on the challenge of diagnosis and treatment. Clinical and Molecular Hepatology, 22(3): 327–335. DOI: 10.3350/cmh.2016.0049
- Zelber-Sagi S., Ratziu, V. & Oren, R. (2011). Nutrition and physical activity in NAFLD: an overview of the epidemiological evidence.World Journal of Gastroenterology, 17 (29):3377-89. DOI: 10.3748/wjg.v17.i29.3377
- The National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. (2016). Treatment of NAFLD and NASH. Retrieved from https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/treatment
- Xiao,J., Kwok, F.S., Liong, E.C. & Tipoe, G.L. (2013). Recent Advances in the Herbal Treatment of Non-Alcoholic Fatty Liver Disease. Journal of Traditional and Complementary Medicine, 3(2): 88–94. DOI: 10.4103/2225-4110.110411
- Doulberis, M., Kotronis, G., Gialamprinou, D., Kountouras, J. & Katsinelos, P. (2017). Non-alcoholic fatty liver disease: An update with special focus on the role of gut microbiota. Metabolism, 71:182-197. DOI: 0.1016/j.metabol.2017.03.013

